Periodontal Disease Causes, Treatment, and Prevention
Gum disease, also known as periodontal disease, is an infection of the gums surrounding your teeth. Gum disease is one of the top reasons for tooth loss in adults, and because it is virtually pain-free, many patients do not know they have the disease. During each regular checkup, your dentist will check for signs of periodontal disease by measuring the space between your teeth and gums.

Periodontal disease is diagnosed by your dentist or dental hygienist during a periodontal examination. This type of exam should always be part of your regular dental check-up.
A periodontal probe (small dental instrument) is gently used to measure the sulcus (pocket or space) between the tooth and the gums. The depth of a healthy sulcus measures three millimeters or less and does not bleed. The periodontal probe helps indicate if pockets are deeper than three millimeters. As periodontal disease progresses, the pockets usually get deeper.
Your dentist or hygienist will use pocket depths, amount of bleeding, inflammation, tooth mobility, etc., to make a diagnosis that will fall into a category below:
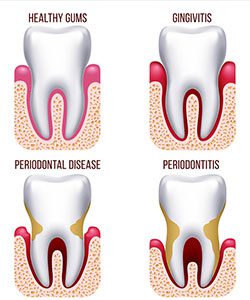
GINGIVITIS
Gingivitis is the first stage of periodontal disease. Plaque and its toxin by-products irritate the gums, making them tender, inflamed, and likely to bleed.
PERIODONTITIS
Plaque hardens into calculus (tartar). As calculus and plaque continue to build up, the gums begin to recede from the teeth. Deeper pockets form between the gums and teeth and become filled with bacteria and pus. The gums become very irritated, inflamed, and bleed easily. Slight to moderate bone loss may be present.
ADVANCED PERIODONTITIS
The teeth lose more support as the gums, bone, and periodontal ligament continue to be destroyed. Unless treated, the affected teeth will become very loose and may be lost. Generalized moderate to severe bone loss may be present.
It only takes twenty four hours for plaque that is not removed from your teeth to turn into calculus (tartar)! Daily home cleaning helps control plaque and tartar formation, but those hard to reach areas will always need special attention.
Once your periodontal treatment has been completed, your dentist and dental hygienist will recommend that you have regular maintenance cleanings (periodontal cleanings), usually four times a year. At these cleaning appointments, the pocket depths will be carefully checked to ensure that they are healthy. Plaque and calculus that is difficult for you to remove on a daily basis will be removed from above and below the gum line.
In addition to your periodontal cleaning and evaluation, your appointment will usually include:
- Examination of diagnostic x-rays (radiographs): Essential for detection of decay, tumors, cysts, and bone loss.X-rays also help determine tooth and root positions.
- Examination of existing restorations: Check current fillings, crowns, etc.
- Examination of tooth decay: Check all tooth surfaces for decay.
- Oral cancer screening: Check the face, neck, lips, tongue, throat, cheek tissues, and gums for any signs of oral cancer.
- Oral hygiene recommendations: Review and recommend oral hygiene aids as needed. (Electric toothbrushes, special periodontal brushes, fluorides, rinses, etc.)
- Teeth polishing: Remove stain and plaque that is not otherwise removed during tooth brushing and scaling.
Good oral hygiene practices and periodontal cleanings are essential in maintaining dental health and keeping periodontal disease under control!
Treatment Options
If you’ve been diagnosed with gum disease, there are a variety of treatment options depending on the details of your situation and the severity of the problem. We always start with the least invasive options, which are non-surgical. However, in more serious cases, surgery may be necessary.
Non-surgical treatment
The first line of defense against gum disease is a unique type of cleaning called “scaling and root planing.” In this procedure, an ultrasonic cleaning device is used to remove plaque and tartar from your teeth where regular cleaning devices can’t reach: under the gum line, on the tooth, and around the root. Then, the rough surface of the tooth and the root are smoothed out (planed). This provides a healthy, clean surface that makes it easier for the gum tissue to reattach to the tooth.
If you address your gum disease before it becomes severe, scaling and root planing may be the only treatment you need. However, as with any dental procedure, after-care is vital. In order to keep your teeth in good shape and resist future occurrences of gum disease, you must brush and floss daily, eat a healthy diet, avoid tobacco use, and have regular dental checkups. Even after a successful scaling and root planing, if you don’t attend to your teeth properly, it’s quite likely that you’ll develop gum disease again.
Surgical treatment options
If the tissue or bone surrounding your teeth is too damaged to be repaired with non-surgical treatment, several surgical procedures are available to prevent severe damage and to restore a healthy smile. We will recommend the procedure that is best suited to the condition of your teeth and gums. Following is a list of common types of periodontal surgery:
- Pocket Depth Reduction
In a healthy mouth, the teeth are firmly surrounded by gum tissue and securely supported by the bones of the jaw. Periodontal disease damages these tissues and bones, leaving open spaces around the teeth that we call pockets. The larger these pockets are, the easier it is for bacteria to collect inside them, leading to more and more damage over time. Eventually the supportive structure degrades to the point that the tooth either falls out or needs to be removed.During pocket reduction procedures (also known as “flap surgery”), we fold back the gum tissue and remove the bacteria hiding underneath, as well as the hardened plaque and tartar that have collected. We may also remove any tissue that is too damaged to survive. We then sew the healthy tissue back into place. Now that the tooth and root are free of bacteria, plaque, and tartar, and the pockets have been reduced, the gums can reattach to the teeth. - Regeneration
When the bone and tissue supporting the teeth have been lost due to severe gum disease, we can restore these areas with a regeneration procedure. During this process, we begin by folding back the gum tissue and removing the bacteria, plaque, and tartar. Depending on your situation, we may then perform a bone graft to stimulate new bone growth, or we may apply a special kind of protein that stimulates tissue growth to repair the areas that have been destroyed by the disease. - Soft-Tissue Graft
A frequent symptom of gum disease is gum recession (also called gingival recession). As the gums recede, more of the roots are revealed. This can make teeth appear longer and can also create sensitivity to hot or cold liquids or food. It also exposes the tooth to increased damage from gum disease, as bacteria, plaque, and tartar attack the surface of the tooth and the root.During a soft-tissue graft, tissue from the top of your mouth or another source is sewed to the gum area, covering the roots and restoring the gum line to its original, healthy location. This procedure can also be performed for cosmetic reasons.
The term “periodontal”means “around the tooth.” Periodontal disease (also known as periodontitis and gum disease) is a common inflammatory condition which affects the supporting and surrounding soft tissues of the tooth; also the jawbone itself when in its most advanced stages.
Periodontal disease is most often preceded by gingivitis which is a bacterial infection of the gum tissue. A bacterial infection affects the gums when the toxins contained in plaque begin to irritate and inflame the gum tissues. Once this bacterial infection colonizes in the gum pockets between the teeth, it becomes much more difficult to remove and treat. Periodontal disease is a progressive condition that eventually leads to the destruction of the connective tissue and jawbone. If left untreated, it can lead to shifting teeth, loose teeth and eventually tooth loss.
Periodontal disease is the leading cause of tooth loss among adults in the developed world and should always be promptly treated.
When left untreated, gingivitis (mild gum inflammation) can spread to below the gum line. When the gums become irritated by the toxins contained in plaque, a chronic inflammatory response causes the body to break down and destroy its own bone and soft tissue. There may be little or no symptoms as periodontal disease causes the teeth to separate from the infected gum tissue. Deepening pockets between the gums and teeth are generally indicative that soft tissue and bone is being destroyed by periodontal disease.
Types of Periodontal Disease
When left untreated, gingivitis (mild gum inflammation) can spread to below the gum line. When the gums become irritated by the toxins contained in plaque, a chronic inflammatory response causes the body to break down and destroy its own bone and soft tissue. There may be little or no symptoms as periodontal disease causes the teeth to separate from the infected gum tissue. Deepening pockets between the gums and teeth are generally indicative that soft tissue and bone is being destroyed by periodontal disease.
Here are some of the most common types of periodontal disease:
- Chronic periodontitis – Inflammation within supporting tissues cause deep pockets and gum recession. It may appear the teeth are lengthening, but in actuality, the gums (gingiva) are receding. This is the most common form of periodontal disease and is characterized by progressive loss of attachment, interspersed with periods of rapid progression.
- Aggressive periodontitis – This form of gum disease occurs in an otherwise clinically healthy individual. It is characterized by rapid loss of gum attachment, chronic bone destruction and familial aggregation.
- Necrotizing periodontitis – This form of periodontal disease most often occurs in individuals suffering from systemic conditions such as HIV, immunosuppression and malnutrition. Necrosis (tissue death) occurs in the periodontal ligament, alveolar bone and gingival tissues.
- Periodontitis caused by systemic disease – This form of gum disease often begins at an early age. Medical condition such as respiratory disease, diabetes and heart disease are common cofactors.
Treatment for Periodontal Disease
There are many surgical and nonsurgical treatments the periodontist may choose to perform, depending upon the exact condition of the teeth, gums and jawbone. A complete periodontal exam of the mouth will be done before any treatment is performed or recommended.
Here are some of the more common treatments for periodontal disease:
- Scaling and root planing – In order to preserve the health of the gum tissue, the bacteria and calculus (tartar) which initially caused the infection, must be removed. The gum pockets will be cleaned and treated with antibiotics as necessary to help alleviate the infection. A prescription mouthwash may be incorporated into daily cleaning routines.
- Tissue regeneration – When the bone and gum tissues have been destroyed, regrowth can be actively encouraged using grafting procedures. A membrane may be inserted into the affected areas to assist in the regeneration process.
- Pocket elimination surgery – Pocket elimination surgery (also known as flap surgery) is a surgical treatment which can be performed to reduce the pocket size between the teeth and gums. Surgery on the jawbone is another option which serves to eliminate indentations in the bone which foster the colonization of bacteria.
- Dental implants – When teeth have been lost due to periodontal disease, the aesthetics and functionality of the mouth can be restored by implanting prosthetic teeth into the jawbone. Tissue regeneration procedures may be required prior to the placement of a dental implant in order to strengthen the bone.
